Beck Depression Inventory Complete Scoring Guide
February 7, 2026 | By Daphne Wells
Waking up with a heavy chest or feeling disconnected from your daily routine can be incredibly confusing. The Beck Depression Inventory is a structured assessment designed to translate these vague emotional struggles into clear, objective data. Rather than leaving you to guess whether you are just going through a rough patch, this tool acts as a mirror to help you understand your mental health status.

This uncertainty is where standardized screening becomes valuable. By understanding how this "gold standard" tool works, you can move from a place of doubt to clarity. This guide explains exactly how the inventory functions, how to interpret its scoring, and how to use a depression screening tool to take the first step toward feeling better.
What Is the Beck Depression Inventory?
The Beck Depression Inventory is one of the most widely used psychometric tests for measuring the severity of depression. Created by Dr. Aaron T. Beck in 1961, it revolutionized how mental health professionals viewed depressive disorders. Before this tool, depression was often seen as a mysterious concept rooted solely in the unconscious mind. Dr. Beck changed the conversation by focusing on the patient's immediate thoughts and perceptions.
Origins and Cognitive Theory
Dr. Beck observed that his patients often expressed negative thoughts about themselves, the world, and the future. This pattern is known as the "cognitive triad." The inventory was designed to measure these specific cognitive distortions.
Instead of guessing, the test asks you to report exactly how you feel right now. For someone feeling overwhelmed, knowing that there is a scientific method to measure these feelings can bring a sense of relief. It validates that your experience is real.
Purpose: Screening vs. Diagnosis
It is crucial to understand that the BDI is a screening instrument, not a diagnostic tool. A high score suggests significant symptoms associated with depression, but it does not replace a doctor's evaluation. Think of it as a thermometer: it can tell you that you have a fever, but it cannot tell you exactly what infection is causing it. Its primary goal is to help you and healthcare providers spot patterns.
Structure of the BDI Content and Time Frame
When you review the Beck Depression Inventory questions, you are engaging with a structured review of your emotional landscape rather than answering random queries.
The 21 Symptom Categories
The test consists of 21 groups of statements. Each group focuses on a specific symptom common to depression. These cover a wide range of human experiences:
- Emotional: Sadness, guilt, feelings of punishment, loss of pleasure.
- Cognitive: Pessimism, self-dislike, suicidal thoughts, indecisiveness.
- Physical: Changes in sleep patterns, fatigue, appetite changes, loss of energy.
The Past Two Weeks Time Frame
The BDI specifically asks you to describe how you have been feeling for the past two weeks, including today. This time frame is critical because clinical depression is generally defined by symptoms that persist for at least this duration. It helps distinguish between a fleeting bad mood and a persistent emotional state.
The 0–3 Severity Scale Per Item
For each of the 21 categories, you select one statement that best describes you. These are scored on a scale of 0 to 3:
- 0: Normal or neutral feeling.
- 1: Mild concern.
- 2: Moderate concern.
- 3: Severe concern.
For example, in the category of "Sadness," a 0 might indicate you don't feel sad, while a 3 might indicate you are so unhappy that you cannot stand it.
BDI vs BDI-II Understanding the Key Differences
If you are researching the Beck Depression Inventory, you will likely see references to the BDI-II. This is the second edition, published in 1996, and is the version most commonly used today.
Why the Update?
The original BDI was groundbreaking, but psychological understanding has evolved. The BDI-II was developed to align more closely with the Diagnostic and Statistical Manual of Mental Disorders (DSM). This ensures that the symptoms being measured match the clinical criteria doctors use to diagnose depressive disorders.
Changes in Symptom Focus
The update made significant changes to physical symptom questions. The original version focused heavily on weight loss and loss of appetite. However, many people experience increased appetite and weight gain when depressed. The Beck Depression Inventory II adjusts for this by asking about changes in appetite or sleep, making it a more accurate reflection of diverse experiences.
BDI Scoring Guide What Do the Results Mean
Once the 21 questions are answered, the values are summed up to create a total score. Below is the standard Beck Depression Inventory scoring guide used to interpret these results.
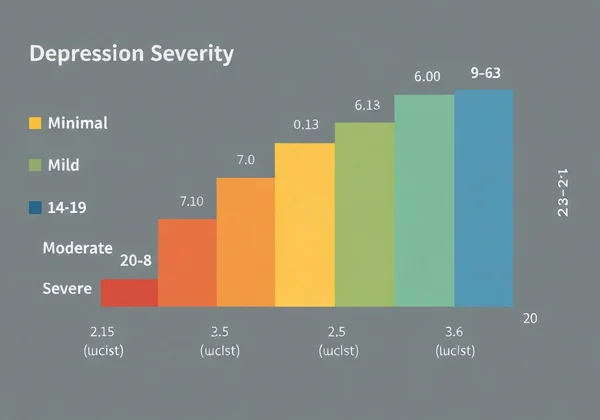
How to Calculate the Total Score
To get your score manually, simply add up the numbers (0, 1, 2, or 3) corresponding to the statements chosen for each item. The lowest possible score is 0, and the highest possible score is 63.
Interpretation Table
| Total Score | Depression Severity | What This May Mean For You |
|---|---|---|
| 0 – 13 | Minimal / Normal | You are likely experiencing normal ups and downs with few distinct symptoms. |
| 14 – 19 | Mild Depression | You may feel consistently low. Daily tasks might feel slightly harder than usual. |
| 20 – 28 | Moderate Depression | Symptoms are likely impacting your quality of life, focus, or sleep. |
| 29 – 63 | Severe Depression | You are likely experiencing intense distress. Professional support is strongly recommended. |
Minimal Range (0–13)
A score in this range suggests that you are not currently showing clinical signs of depression. However, if you scored high on specific items like hopelessness, those individual symptoms are still worth addressing.
Mild to Moderate Depression (14–28)
Scores here indicate that something is weighing on you. You might be functioning at work or school, but it takes significantly more effort than it should. This is often the time when self-care and support strategies are most effective.
Severe Depression (29–63)
A score in this range is a loud signal from your mind and body that you are carrying a heavy burden. It validates that your struggle is severe and that you deserve professional support to help lift the weight.
Where to Take a Depression Assessment Online
Understanding the scoring mechanics is helpful, but manually calculating results can be tedious. In a moment of vulnerability, the last thing you want to do is math.
Manual Calculation vs. Automated Analysis
Manually taking the Beck Depression Inventory carries a risk of calculation error. Furthermore, a raw number like "24" tells you severity but doesn't explain context. It fails to identify which specific areas of your life are taking the biggest hit.
Why Choose an AI-Powered Report
Modern digital tools have evolved beyond simple scoring. By using an automated depression test, you can bypass the manual work. Our platform uses clinical principles similar to the BDI but enhances them with instant analysis. You receive personalized insights into your symptom clusters immediately, ensuring your results are private and actionable.
Accuracy and Limitations Is the BDI Reliable
When you see your results, a common reaction is skepticism. It is important to know the strengths and weaknesses of this tool.
High Validity as a Screening Instrument
Research consistently shows that the Beck Depression Inventory scale has high validity. It correlates well with biological and clinical symptoms. If the BDI says you are reporting high levels of distress, you likely are. It remains one of the most trusted tools globally.
Limitations of Self-Reporting
However, the test relies entirely on self-reporting. You might downplay symptoms to avoid feeling "weak," or over-report during an exceptionally bad day. Additionally, the test cannot know if you have a medical condition that mimics depression, such as thyroid issues. Therefore, Beck Depression Inventory interpretation should ultimately be discussed with a professional.
Taking the Next Step for Your Mental Health
Seeing a high score can feel frightening, but it can also be empowering. It transforms a vague cloud of "feeling bad" into a concrete problem that can be solved.
A high score is a snapshot of your current state, not a life sentence. Whether you use a paper form or a digital tool, keep a copy of your results to show a therapist. If your numbers indicate moderate or severe distress, consider reaching out to a professional. If you are ready to stop guessing, you can assess your emotional well-being right now with our free, private online tool.
Frequently Asked Questions
Is the Beck Depression Inventory free to use online?
The original BDI and BDI-II are copyrighted materials owned by Pearson Assessment. While the official clinical version requires a license, many free online screening tools are based on similar validated clinical principles to provide accessible self-assessment for users.
How long does it typically take to complete the BDI?
The test is designed to be quick and efficient. Most people can complete the 21 questions in approximately 5 to 10 minutes, making it an accessible first step for checking mental health.
Can the BDI be used for adolescents or teenagers?
The standard BDI-II is generally suitable for individuals aged 13 and older. However, interpreting scores for teenagers requires care due to natural emotional volatility. Specific tools like the Beck Depression Inventory for Youth are often better for younger populations.
Is a high score on the BDI a medical diagnosis?
No, a high score indicates a burden of depressive symptoms but is not a medical diagnosis. Only a qualified healthcare professional can diagnose Major Depressive Disorder after a comprehensive evaluation that rules out other potential causes.
What are the recommended next steps after receiving a high score?
If your results indicate moderate to severe depression, the recommended step is to consult a mental health professional. They can use your results as a starting point to discuss treatment options, such as therapy, lifestyle changes, or medication.
How does the BDI compare to scales like the PHQ-9?
The PHQ-9 is shorter and maps directly to DSM diagnostic criteria, while the BDI is longer and provides more detailed nuance regarding symptom severity. Both are excellent, reliable screening tools widely used in clinical and research settings.